Day 1 :
Keynote Forum
Nelson Hendler
Evaluating chronic pain patients using methods from Johns Hopkins Hospital physicians
Keynote: Evaluating chronic pain patients using methods from Johns Hopkins Hospital physicians
Time : 10:00-10:30

Biography:
Nelson Hendler has graduated cum laude from Princeton University. He has an MD and MS in Neurophysiology from University of Maryland School of Medicine. He did his Residency in Psychiatry at Johns Hopkins Hospital and remained as the Faculty at the Medical School for 31 years. He has published 4 books, 33 medical text book chapter, and 65 articles. He has lectured in over 60 hospitals and medical schools in the US and in 10 other countries. He has served as the President of the American Academy of Pain Management and the Reflex Sympathetic Dystrophy Association of America and served on the board of the Lightning Strike and Electric Shock Survivors International.
Abstract:
Chronic pain patients are misdiagnosed 40%-80% of the time, according to research from Johns Hopkins Hospital physicians. The most common of these misdiagnoses is sprains or strains, which are listed in medical textbooks as self-limited disorders, which resolve in less than three weeks without treatment. Yet these diagnoses account for over 50% of diagnoses in patients with pain for more than three months. On the other hand, certain diagnoses are overused, and misapplied without attention to published diagnostic criteria. Therefore, complex regional pain syndrome (CRPS) formerly called reflex sympathetic dystrophy (RSD), and fibromyalgia, are over diagnosed 71% to 97% of the time, to the detriment of the patients. The leading causes of these errors in diagnoses are: failure to take a complete history and using the wrong medical tests. As an example, MRIs fail to detect damaged discs 78% of the time compared to a provocative discogram, and CT fail to detect bony lesions 56% of the time compared to 3D-CT. Two expert system internet questionnaires are discussed. The pain validity test predicts the presence of abnormal medical testing with 95% accuracy, which validates the complaint of pain, and detects drug seeking behavior. Another internet based expert system the diagnostic paradigm, provides diagnoses with a 96% correlation with diagnoses of Johns Hopkins Hospital physicians. The associated treatment algorithm recommends the appropriate tests to use for confirm the correct diagnosis. The value of these two systems is documented by published outcome studies, which demonstrate patient improvement rates far higher than other methods. These publications report cost savings $20,000 to $175,000 a case, with an 89% reduction in narcotic use, and a 45% reduction in doctor visits. Between 50%-63% of patients need surgery to improve.
Keynote Forum
Jeff L. Xu
Westchester Medical Center & New York Medical College, USA
Keynote: Paraneuraxial nerve blocks: Can they replace neuraxial nerve blocks?
Time : 10:30-11:00

Biography:
Jeff L Xu is a Chief of Regional Anesthesia & Acute Pain Management, Program Director of Regional Anesthesia & Acute Pain Medicine Fellowship. As the founder of the Regional Anesthesia & Acute Pain Services at Westchester Medical Center, he initiated and developed the regional anesthesia program for the anesthesia residents. He also is the founder of the fellowship program for Regional Anesthesiology & Acute Pain Medicine at Westchester Medical Center, New York medical College, USA, and served as Fellowship Program Director. He also served as Principal Investigator on multiple clinical studies, speaker for regional anesthesia workshops, and reviewer for peer review journals.
Abstract:
Over the past 10 years, the introduction of ultrasound has rapidly changed the practice of regional anesthesia including the greater use of truncal nerve blocks. In the truncal block family, some of the blocks are performed just outside of neuraxial region, such as paravertebral nerve block (PVB) and lumbar plexus block, in addition to thoracolumbar interfascial plane (TLIP), retrolaminar block (RLB), erector spinae plane (ESP) block, and cervical columnar interfascial plane (CLIP) block, which are new techniques. These techniques are comparable to neuraxial nerve blocks in terms of success rate and analgesic efficacy and may confer many of advantages over neuraxial nerve blocks. Specifically, neuraxial blocks are not site-specific, they cause hypotension, and some of them may lead urinary retention, the placement of Foley catheters, limited mobility. Furthermore, neuraxial nerve block, such as epidural, was limited on patient who has spine fracture, spine instability, spine surgery or sepsis. Instead, paravertebral nerve block, most recently, has been performed more often clinically. In addition, most of the truncal techniques can be performed in fully anesthetized patients, pronounced hypotension is unusual as sympathetic blocks are rarely bilateral, and urinary retention does not occur. We have proposed the use of the new terminology paraneuraxial nerve block. This new term provides a direct pictorial anatomy of the nerve block and would help clinicians develop clinical insights. This term has never been well-defined either anatomically or clinically. Anatomically, the paraneuraxial nerve is the spinal nerve between the lateral margin of the spinal foramen and the lateral edge of the erector spinae muscle. It contains the roots of the spinal nerve and its dorsal and ventral branches and their plexuses, white and gray rami communicantes, the sympathetic ganglion, and the sympathetic chain. The paraneuraxial nerve block family may include (but is not necessarily limited to) the PVB and the lumbar plexus nerve block, as well as ESP, RLB, TLIP block, CLIP block, sympathetic chain block. We believe that paraneuraxial nerve block will become even more popular clinically, due to its clinical and anatomical characteristics. It is thus clinically significant and beneficial in the practice, teaching, and training aspects of regional anesthesia. Study has shown that since 1990, wherein the relative percentage of spinal and epidural techniques has declined, and peripheral nerve blocks have increased. Paraneuraxial nerve blocks will challenge the clinical role of the traditional neuraxial nerve blocks fundamentally.
Keynote Forum
William P Gallagher Jr
American Academy of Motor Vehicle Injuries, USA
Keynote: Understanding the mechanism of injury: A means to provide better direction for proper diagnoses in motor vehicle collisions
Time : 11:25-11:55

Biography:
William P Gallagher Jr. has practiced chiropractic in Arizona and California for the past 30 years. As someone who has survived several motor vehicle collisions, this is an area of particular concern to him. In order to learn and teach about motor vehicle injuries he created the American Academy of motor vehicle injuries. The academies 150 hour certificate program teaches doctors how to diagnose, document, and manage a personal injury case. Half of the core curriculum is on exam and diagnosis and all of that is based on understanding first the mechanism of injury. He publishes a personal-injury quarterly for the Arizona Association of chiropractic and is a contributing Editor to attorney at law magazine.
Abstract:
Statement of the Problem: Diagnosing any disease or injury can be a challenge even for the most experienced physicians. Studies dating back to the 1999 Institute of Health report, To Err is Human estimated up to 98,000 die each year in the US due to medical errors and to death by medicine in 2011 that calculated 784,936 deaths, making medical errors the leading cause of death in the US. Unfortunately, the all too common lack of proper diagnosis not only exposes the doctor to malpractice but it also leaves the patient with inappropriate treatment and quite often a failure to recover. With motor vehicle collisions, understanding the mechanism of injury is an essential tool toward a better diagnosis.
Literature Review: Past studies with live subjects offer a better understanding of spinal motion and what structures can be injured. Unfortunately, knowing the probability of injury it is difficult to do additional live testing today to observe injuries that were overlooked in past studies. This is of particular concern with concussions/traumatic brain injuries that until recently were commonly overlooked. Testing on these injuries today is primarily with athletes and military personnel with little information on motor vehicle collisions. What we lack in knowledge of the mechanism of injury becomes evident in our failure to diagnose so many conditions.
Conclusion & Significance: Live subject studies can in part be replaced by digital modeling. Coupled with existing knowledge of biomechanics this can be a useful resource. For the most part the ability to diagnose injuries still goes back to the basic foundation of a good history. Understanding the mechanism of injury is an essential starting point for that history and in turn the means to a better diagnosis.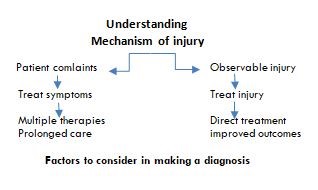
Keynote Forum
Peter W. Schiller
University of Montreal, Canada
Keynote: Bi- or multifunctional opioid analgesics
Time : 11:55-12:25

Biography:
Peter W. Scihiller is a Medicinal Chemist and Pharmacologist. He is a research Professor in the Department of Pharmacology and Physiology of the University of Montreal and at the Montreal Clinical Research Institute (Canadian Pacific Chair in Pain Research). His research in the opioid field resulted in the discovery of highly receptor-specific agonists and antagonists and of opioids with novel bi-or multifunctional activity profiles. Some of his compounds are widely used as pharmacological tools or are being pursued as analgesic drug candidates. He has published over 400 scientific articles and holds 17 patents. He was elected Fellow of the Royal Society of Canada (Academy of Science) and of the American Association for the Advancement of Science (AAAS). His numerous awards include the Prix Galien of Canada for excellence in pharmaceutical research, a NIH MERIT Award and the Vincent du Vigneaud Award from the American Peptide Society.
Abstract:
Acute pain typically responds well to treatment with opioids and NSAIDs, whereas neuropathic pain is difficult to treat with only 40-60% of patients achieving pain relief. Currently used treatments, including tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, anticonvulsants and morphine are either ineffective or produce major, limiting side effects. Our goal is to develop opioids with novel bi- or multifunctional activity profiles for treatment of chronic pain with minimal side effects. [Dmt1]DALDA (SS-02), a tetrapeptide with excellent drug-like properties, is a potent mu opioid analgesic and also is a mitochondria-targeted antioxidant. Mitochondrial reactive oxygen species (ROS) play a key role in mechanisms of neuropathic pain and there is evidence that ROS quenchers synergize with opiates in alleviating neuropathic pain. As expected, SS-02 turned out to be more effective than morphine in a rat model of neuropathic pain. Similarly, in a rat model of complex regional pain syndrome (CRPS-1), SS-02 and one of its analogues produced an up to 70-fold more potent and longer-lasting analgesic effect as compared to morphine. A structurally related peptide (SS-20) capable of promoting mitochondrial energetics had a protective effect against the development of chemotherapy-induced peripheral neuropathy in mice. Thus, these compounds are excellent drug candidates for neuropathic pain treatment. In a different approach we developed bifunctional compounds that target two distinct receptors. On the basis of a strong pharmacological rationale compounds were designed that act as agonists at the mu opioid receptor (MOR) and as antagonists at the delta opioid receptor (DOR). Such MOR agonist/DOR antagonists turned out to be potent analgesics in the rat tail flick test with low propensity to produce analgesic tolerance and dependence. Furthermore, bifunctional MOR agonist/NK1 receptor antagonists and opioid agonist/nociceptin antagonists were more potent than morphine in a neuropathic pain model and in one case did not produce respiratory depression.
- Pharmacological Approaches for Pain | Anesthesiology and Pain Medicine | Interventional Pain Management Pain Management and Rehabilitation | Pain Management Market | Non-Pharmacological Approaches for Pain
Location: Brussels

Chair
Nelson Hendler
Johns Hopkins University School of Medicine, USA

Co-Chair
William P Gallagher Jr
American Academy of Motor Vehicle Injuries, USA
Session Introduction
Sigal Meilin
MD Biosciences, Israel
Title: Peripheral nerve trauma in the pig, a model for neuropathic pain: Evaluation of the evoked and spontaneous pain
Time : 12:25-12:50

Biography:
Sigal Meilin has passion over 20 years in the understanding of neuro-degeneration and pain processes. Her research focus has been on exploring and creating models of pain including translational models in post incision wounds in pigs which closely mimics humans’ condition. She holds a PhD from Bar Ilan University in Tel Aviv, Israel where she continued her research involving multi-parametric monitoring of the living brain and the cross talk between the immune system and the neuronal system in neurodegenerative disease. She was the Leader of the Pharmacology Department of Pharmos Ltd, prior to joining MD Biosciences in 2006.
Abstract:
Rodent models are frequently used in the research of pain and continue to provide valuable data on the mechanisms driving pain although criticized due to limited translation ability to human conditions. Previously we have suggested expressed mechanical and tactile allodynia, indicative of painful neuropathy 28 post-surgery peripheral nerve traumas (PNT). In this study we investigate the spontaneous behavior of the pigs following PNT induced neuropathic pain. Computerized monitoring system was used to evaluate the changes in the open field test in addition to a applying a composite behavior scoring system. The data suggest the PNT operation did not affect the animal’s ability to walk as the total distance walked by PNT animals was not different than the total distance walked by Sham operated animal. However, PNT animals expressed a significant change in pattern alteration. This effect was unrelated to the time that the animals spent in the open field. Following treatment with different drugs (Morphine, Buprenorphine or Gabapentin) the walking pattern of the animals in the open field changed in a drug specific manner. Also, the detailed behavior score revealed drug specific changes following treatment. Pharmacokinetic analysis of the 3 tested drugs blood and CSF concentration was correlated with the behavior analysis. Over all the data of this study suggest that the open field test together with the detailed behavior score applied in this model are a very powerful tool to assess the spontaneous behavior of pigs following PNT induced neuropathic pain.
Matthias Seidel
Pain Clinic Basel, Switzerland
Title: Neurogenic information in autoimmune diseases and chronic pain syndromes
Time : 13:50-14:15

Biography:
Matthias Seidel has obtained his graduate medical and neuroscience training in Italy, Germany and the United States. He received his medical degree in Essen (Germany) and then served as a Marie-Curie-Fellow in Créteil (Paris/France). He is licensed in Internal Medicine and Rheumatology and has worked in several rheumatology departments in Bonn (Germany), Basel and Biel/Bienne (both Switzerland) where he was recently appointed a chief position. His major scientific interests are neurogenic inflammation in clinical medicine, biomarker molecules and rare diseases in rheumatology.
Abstract:
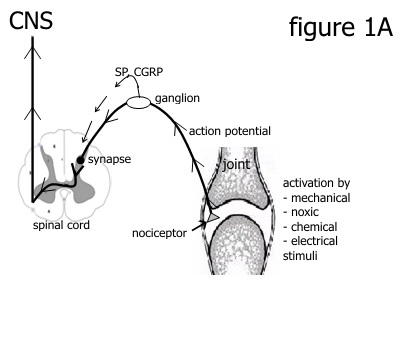
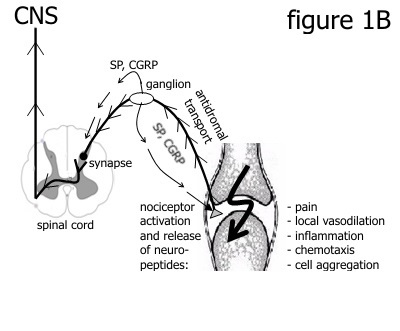
Pain is a key symptom in many musculoskeletal diseases. Persistent nociceptor stimulation activates the peripheral and central nervous system (figure 1A, 1B)), and induces the release of neurotransmitters such as substance P (SP) or calcitonin-gene related peptide (CGRP). Such molecules mediate peripheral tissue inflammation with reddening, swelling, hyperalgesia or allodynia (1). These events are termed neurogenic inflammation (NI). Nerve growth factor (NGF) is a primary stimulator of SP and CGRP. A variety of degenerative and autoimmune inflammatory diseases are characterized by NI and either show a robust upregulation of neuronal mediators or clinical features of disease exasperation after stimulation of the nervous system (2). The latter include internal or external Köbner phenomenon in psoriatic arthritis, pathergy in Behçet’s disease, UV light-induced dermatitis in systemic lupus erythematosus or chronic regional pain syndrome (CRPS) that is typically induced by trauma. Further strong evidence for NI in musculoskeletal diseases is provided by clinical trials with molecules that block neuron-derived molecules. Recently, erenumab has been approved for the treatment of chronic migraine (3). This monoclonal antibody binds to the CGRP receptor. Treatment with monoclonal antibodies against NGF such as tanezumab (4) or fasinumab (5) have been effective in chronic pain syndromes including osteoarthritis or low back pain. In conclusion, NI is now more increasingly recognized as an important mechanism in clinical medicine.
|
|
Lene Moeller Schear Mikkelsen
National University Hospital, Denmark
Title: Complex Regional Pain Syndrome (CRPS): Rehabilitation and interdisciplinary treatment– seen from a rehabilitation based therapy approach
Time : 14:15-14:40
Biography:
Lene Møller Schear Mikkelsen, PT, completed her Master in Rehabilitation. She has her expertise in Physical Therapy and Rehabilitation. She is highly skilled in pain management and improving interdisciplinary approach to patients with chronic pain conditions.
Abstract:
Statement of the Problem: The treatment and rehabilitation of patients with CRPS is challenging. The limited knowledge on the pathophysiology and its complex mechanisms contribute to the fact that CRPS is difficult to treat. Often this means that the disease is treated by an individual knowledge, clinical experience and preference of the individual professionals. In many cases, it is without an interdisciplinary and cross-sectoral approach. Often patients with CRPS are faced with multiple consultations and it is perceived that many patients with CRPS in Denmark are diagnosed late in their illness. However there is international consensus on diagnostic criteria and early identification. Evidence for treatment is weak, but there are good experiences with highly specialized interdisciplinary treatment. Rehabilitation based therapy is recommended as the core treatment for CRPS. In view of this, a Danish National Treatment Guideline for CRPS was developed. The rehabilitation based therapy approach described in this guideline was based on a study to identify current practice among clinicians who deliver rehabilitation based therapy to patients with CRPS.
Methodology: An online survey was disseminated to physio- and occupational therapists who works with CRPS in Denmark. Responders were asked about which kind of treatment they found useful, outcome measures, and challenges related to the course of treatment.
Findings: Within this survey, the physio- and occupational therapists emphasized the importance of an interdisciplinary approach and called for a function-based treatment algorithm so patients are offered a more uniform treatment due to clinical and evidence-based practice.
Conclusion & Significance: CRPS is a multifactorial condition and should be treated as such by a specialized interdisciplinary team. Applicable to the therapeutic part of the National Treatment Guideline for CRPS a function-based treatment algorithm was developed. This survey was the first step trying to develop a best practice model of a therapeutic based approach.
Ali Alqahtani
Orthopain Center, Kingdom of Saudi Arabia
Title: Which is challenging? chronic pain or chronic pain education/training; Bringing the innovative solution into medical education, research and practice
Time : 14:40-15:05

Biography:
Ali Hasan Alqahtani, from Saudi Arabia. consultant Chronic Pain and Musculoskeletal Medicine. He has obtained the Canadian fellowship in chronic pain/musculoskeletal medicine in 2010 from McMaster University ,and double board Family Medicine from National Guard Medical City in 2000. He have created a new fellowship at McMaster University that combines pain and musculoskeletal Medicine from the perspective of anaesthesia, physiatry, sport medicine, podiatry, pain psychiatry, pain psychology, palliative med., regenerative med, and complementary/alternative pain medicine. The main goal was to fill the gaps in knowledge, skills, researches, education and legislation. He was the first graduate from this 30 months fellowship. It was recognized ,by CAPM and McMaster University ,As the most extensive and most comprehensive training in Canada, which included extensive literature review of the past 30 years literatures from different perspectives. He has implemented the outcomes of this fellowship in KSA since early 2010. He is a primary contributor for a major change in pain services in his country under Ministry of Health. He has established the integrative Chronic Pain Center as a private center in Riyadh after five years of Chronic Pain practice in the largest medical city in KSA, then 4 years in his own center in Riyadh, The first Model/center of its kind in the KSA.
Abstract:
Chronic pain is perceived by physicians and healthcare systems worldwide as a major challenge. It costs USA more than the cost of cancer, cardiovascular diseases, and AIDS. Despite the major efforts to solve this problem, these efforts have gone in the wrong direction. Chronic pain associated knowledge and pain practices are dissociated. Researches, medical education, legislation priorities and directions are influenced by economic dominance. All available medical/surgical specialties dealing with chronic pain can’t see the full picture of the nature and dimensions of chronic pain. Chronic pain is either neuromusculoskeletal, neurovisceral or neuroendocrine dysfunction. A new training/education fellowship had been created at McMaster University in Canada 2007- 2010. This is a 30 months fellowship that included rotations in pain center under anaesthesia, outpatient musculoskeletal physiatry, podiatry, pain psychiatry, neurology, pain psychology, palliative medicine, spinal surgery, sports medicine, complementary/alternative pain medicine. This advanced training/education involved an extensive literature review of the past 30 years of research. The main outcome of this model is an advanced approach to diagnosis and treatment. The main focus is on diagnosing and treating underlying cellular dysfunction and the physical, mental and social dysfunctions using save and cost-effective options. A comprehensive mechanisms specific treatment protocol is used (the RRMMHS protocol) which means:
R: Regenerative, R: Rehabilitative, M: Medication-conventional, M: Mind-body medicine (including psychotherapy), H: Herbal medicine, S: Supplements.
Sajid Rashid
Multan College of Physiotherapy, Pakistan
Title: Awareness and use of ergonomically designed equipment and furniture by public and private sector bankers
Time : 15:05-15:30

Biography:
Sajid Rashid, PhD-PT (HEC Scholar), PP-DPT, MISCP (Ireland) is the Principal/HOD, Multan College of Physiotherapy. He is also a member of Irish Society of Chartered Physiotherapist. He did his graduation in Physical Therapy from King Edward Medical College. He did his MPhil from Riphah University and is currently pursuing his PhD from Isra University. His objective is to make effective use of his experience through serving in a well reputed organization in the field of Physical Therapy and Rehabilitation. He is a reviewer of the journals, Pakistan Journal of Medical Science & Journal of Riphah College of Rehabilitation Sciences. He has several research articles and clinical and teaching experiences. He also attended several workshop and courses. He has vast experience in serving well reputed government and private sector organizations. He worked as a clinician, an academician, a researcher and also an administrator. He has different certificates in medical education and is certified in different techniques. He presented his research work at various national and international forums.
Abstract:
Background & Objective: Neck and shoulder are the most susceptible areas for developing musculoskeletal symptoms among computer users. The modifiable risk factors for these work related musculoskeletal disorders include physical office environment and psychosocial work related factors. Computer workstation layout had been shown to be an important physical aspect of work environment that influences the upper quadrant symptoms. Our objective was to find the frequency of neck and shoulder pain and use of adjustable computer workstation among bankers.
Methods: A cross sectional study was conducted and 120 participants were questioned. Purposive sampling technique was used in this study. Maastricht Upper Extremity Questionnaire (MUEQ) was remodeled and important questions were extracted from its detailed version. The tool was then validated by taking expert opinion. Frequencies and percentages were calculated for categorical variables.
Results: Pain in the neck during working hours was experienced by 71.67% of the respondents and 48.33% of the participants had experienced shoulder pain during working hours. Adjustable keyboards were used by 16.67% of respondents. Back care material was used by 40% bankers. Adjustable chairs were used by 95.83% of the participants. Only 3% of the bankers did not have chairs with adjustable heights. Chairs with adjustable armrests were used by 25% bankers.
Conclusion: Neck and shoulder pain are common occurrences among bankers. Most of the components of workstations of bankers were adjustable but some of them still need attention.
Chan Tak Yin
Hong Kong Public Hospital, Hong Kong
Title: Perspective in pain management using traditional Chinese medicine: East meets west
Time : 15:30-15:55
Biography:
Chan Tak Yin is a Registered Nurse of Hong Kong Public Hospital. She is studying Master of Science in Nursing in the Hong Kong Polytechnic University. She was awarded Sir Edward Youde Memorial Prize in 2002; Outstanding student for CM(N), KCC Award in 2003; Ida Martinson Scholarship for Advanced Nursing Development (Overseas Placement) in 2017 during her school life. She has been to Sun Yat-sen University in Guangzhou for academic exchange and communication in 2016 and awarded Third Prize in the Nursing Researcher Forum. The Ida Martinson Scholarship placement in Florida broadens her horizon and enriched her learning experience in a professional and international context. She had just applied as member of Sigma Theta Tau International.
Abstract:
An exchange of ideas with University of Minnesota students through email, Skype and Facebook communication was done to compare pain management between United States (US) and Hong Kong (HK). There are quite a lot of differences with US people view pain as a weakness with the saying Pain is weakness leaving the body. HK elderly percept pain as essential of aging process, which is a defining characteristic of human life, and it is related to climatic and seasonal conditions to be treated with over-the-counter pain relief patches. Both countries people prefer non-pharmacological approaches first before taking analgesic by hot and cold packs, aromatherapy, humidifier for sore throat used in US; application of medicinal wine or salve, eating preserved fruits such as citrus peel and kumquat for sore throat used in HK. Alternative treatments such as moxibustion are becoming more recognized but slow to be accepted in US with a lack of evidence-based research to support efficacy. In addition, they are not covered by medical insurance. In HK, several charities subsidized Chinese medicine clinics have acupressure and acupuncture specialties to provide trustworthy and inexpensive treatment to people. But moxibustion remains a less popular and recognized therapy, which can be administered easily with moxa stick ignition.
Muhammad Ali Rajput
Multan Medical & Dental College, Pakistan
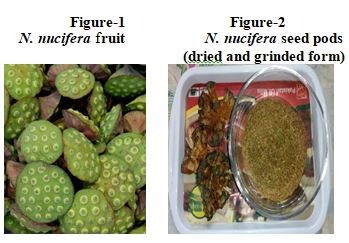
Title: Assessment of analgesic activity of Nelumbo nucifera fruit
Time : 16:15-16:40

Biography:
Muhammad Ali Rajput is a young researcher and Medical Doctor from Pakistan who has attained PhD and MPhil degrees in Pharmacology from University of Karachi, Karachi and MBBS degree from Liaquat University of Medical & Health Sciences Jamshoro, Pakistan. He attended course of Professional Competency Enhancement Program for Teachers (PCEPT) in May 2009 and became certified academician of Higher Education Commission (HEC), Pakistan. He is well oriented with scientific writing and has so far published 9 articles in journals of international repute and many are under peer review process. He has a teaching experience of more than10 years and currently serving in Multan Medical & Dental College as Assistant Professor in the Department of Pharmacology. He is well acquainted and expert in conducting teaching sessions based on either conventional or integrated methods of learning and have conducted MBBS, BDS, DPT and BS nursing classes.
Abstract:
Recently use of herbal therapies and diet rich in flavonoids and vitamins has increased considerably to treat minor to modest inflammatory disorders, thus existing study was focused to evaluate the analgesic effect of Nelumbo nucifera fruit in order to justify its traditional use Pharmacologically in disorders which are associated with pain and inflammation e.g. cancer and arthritis. In current study central analgesic activity in mice was assessed by tail flick test and tail flick latency difference (TFLD) i.e. the time in seconds taken by mouse to remove its tail clearly out of water was noted as the reaction time, Similarly acetic acid induced writhing test was also conducted for the assessment of systemic analgesic effect in mice and number of writhes were counted along with percent inhibition of writhes. Both tests were conducted utilizing separate set of 49 white albino mice of either sex weighing 20-25 g and were equally placed in seven groups. In tail flick test the peek anti-nociceptive effect at all doses of fruit was observed at 90 minutes, however the percentage of tail elongation time was highest at a dose of 200 mg/kg i.e. 82% at 90 minutes. Number of writhes was highly significantly reduced at all doses of N. nucifera fruit but maximum effects were observed at dose 200 mg/kg as compared to control (indicating 48.41 % inhibition of writhes). N. nucifera fruit have exhibited strong analgesic effect in both animal models which was highly comparable with aspirin and that may be connected with the inhibition of arachidonic acid metabolism hence justified its traditional use in disorders associated with pain and thus encourage more preclinical and clinical trials in this field.
Miu Ha Chan
The Hong Kong Polytechnic University, Hong Kong
Title: Abdominal acupuncture - instant painless way to kill pain caused by tissue injury
Time : 16:40-17:05
Biography:
Miu Ha Chan is a Registered Chinese Medicine Practitioner working in University Health Service of The Hong Kong Polytechnic University. Her specialty is in acupuncture and TCM gynecology. She is good at using acupuncture to treat acute and chronic pain caused by muscular skeletal injuries and neuralgia, children developmental retardation; using acupuncture combined with TCM medicine to treat menstruation disorder, infertility, menopausal syndrome, emotions disorder and so on. Abdominal acupuncture is one of her frequent use acupuncture technic to treat acute pain caused by tissue injuries.
Abstract:
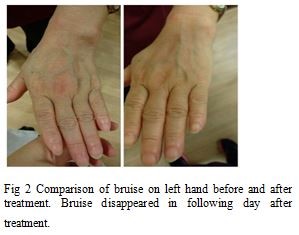
Introduction: Abdominal acupuncture (AA), Bao’s Fu Zhen is a kind of new therapy developed by Prof. Bao Zhi-Yun in China. AA uses the area between CV12 (ZhongWan) and CV3 (ZhongJi) on the vertical line and Sp15 (DaHeng) as the outer most points on the horizontal lines. To cure acute tissue injuries, two typical cases are illustrated.
Case 1 Fall Injury: Ms. Zeng. Zeng fell accidentally during work. Hematoma on left chin and felt pain on left neck, shoulder, arm. Pain increased when doing left shoulder movements. Treatment: CV12, KI19 left, CV10, KI17 bilateral, ST24 left, shoulder and neck corresponding point left, upper rheumatism point (AB1) left, upper lateral rheumatism point (AB2) left with 3 needles, all points are punctured in superficial, depth was about 0.1-0.2 cun. After 20 minutes of treatment, pain improved and swelling reduced.
Case 2 Finger injury: Ms. Chan. Left fingers were clipped by the closing taxi door. Four fingers on left hand were swollen, painful and not able to flex. Left hand was raised up with fingertips pointing upwards, used right index fingertip to massage the upper lateral rheumatism point (AB2, 1 cun laterally from ST 24) on the left upper abdomen gently for 2-3 minutes, pain and swollen dissipated about 50%. Another 10 minutes massaging the point, kept flexion fingers and then flexor fist. Not much pain retained in the injured fingers in the next day.
Conclusion: Abdominal acupuncture, unlike traditional acupuncture, DeQi sensation is not required, once getting the correct points with superficial puncture, the pain on distant injured tissue will cease. Therefore it is a super weapon to kick away pain without pain.

Damien Haton-Pietrin
Neuromodulation Fundamental Physics Laboratory, France
Title: Chronic pain and comorbidity: How to increase the sexual excitation in spinal cord stimulation relief patients over 40 years old?
Time : 17:05-17:30
Biography:
Damien Haton-Pietrin is an Experienced Pain Physician, Mathematician and Physicist. He worked at Interventional Pain Center near Paris before he began a new career as Biophysicist of the central nervous system working especially on the spinal cord diseases.
Abstract:
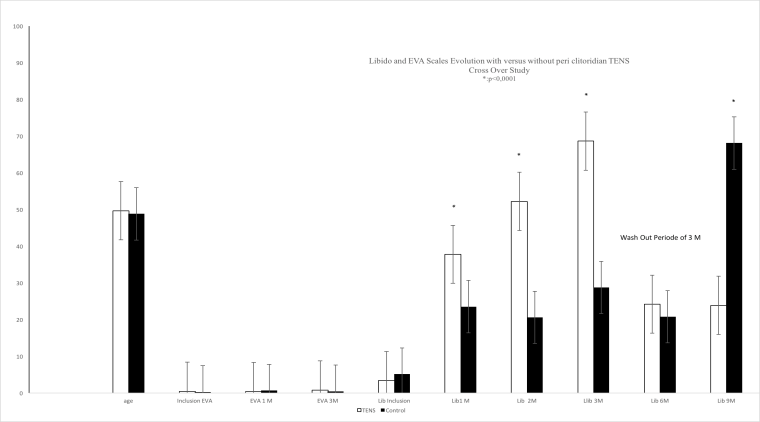
Introduction: Chronic pain causes a drastic reduction in libido that is also physiologically lowered in 40% of women, over 40 years. TENS has never been so far published have an effect on libido. We used TENS for peri clitoral with electrical stimulation 3 V to 6 V for 30 minutes, 3 times a day for three months. The population of women studied was divided into two groups: TENS group was evaluated versus the control. Pain scores EVA was measured, a rated scale of 0 to 100 were used to measure the libido experienced by patients. Inclusion criteria in tested group were: SCS chronic pain relief longer than 3 months and up to 3 years, and the inclusion criteria recommended by the INS for the SCS. Two groups of patients were formed: TENS-C group: TENS for 3 months and then stop (n = 35) versus C-TENS group (n = 22). Both scales were measured according libido and EVA, at baseline of 1, 3, 6 and 9 months. TENS was stopped at three months after inclusion for the treated group. Treated and control group were monitored at 1-2-3-6 and 9 months. A washout period was defined for cross over with a simple observation period of 3 months. Statistical analysis consisted of t-test.
Methods & Results: The population was homogeneous in absence of pain (p>0.5). 33 patients were included in the TENS-C group and 20 patients in the C-TENS group. The results of TENS show that electrical stimulation (ES) of the anterior pelvis promotes a significant increase (p<0.0001) of the libido in the C-TENS group at the first month of treatment. This increase experienced sexual appetence on a numerical scale is constant as long as the treatment is active. Libido in both groups was comparable and not significantly different after the washout period. The C-TENS group also has an increased libido during treatment.
Conclusion: Chronic pain is causing much comorbidity including a drop-in libido which worsens the quality of life of patients. The use of an electrical stimulation device for low voltage shows that the patients treated with TENS feel increased libido. The clearance period also helps to show that the non-treated group initially present after three months of treatment increased libido. In the absence of ES, libido was lowered in the TENS-C group after three months of washout. These results are encouraging for the treatment of comorbidities related to chronic pain which cut the quality of life of female patients over 40 who also suffer the aging of sexual excitability with age.